Introduction
Swine influenza is a highly contagious respiratory disease in pigs caused by one of several swine influenza A viruses. In addition, influenza C viruses may also cause illness in swine. Current strategies to control swine influenza virus (SIV) in animals typically include one of several commercially available bivalent swine influenza virus vaccines.
Transmission of swine influenza viruses to humans is uncommon. However, the swine influenza virus can be transmitted to humans via contact with infected pigs or environments contaminated with swine influenza viruses. Once a human becomes infected, he or she can then spread the virus to other humans, presumably in the same way as seasonal influenza is spread (ie, via coughing or sneezing).
History
The ability to trace outbreaks of swine flu in humans dates back to investigation of the 1918 Spanish influenza pandemic, which infected one third of the world’s population (an estimated 500 million people) and caused approximately 50 million deaths. In 1918, the cause of human influenza and its links to avian and swine influenza was not understood. The answers did not begin to emerge until the 1930s, when related influenza viruses (now known as H1N1 viruses) were isolated from pigs and then humans.1
In humans, the severity of swine influenza can vary from mild to severe. From 2005 until January 2009, 12 human cases of swine flu were reported in the United States. None were fatal. In 1988, however, a previously healthy 32-year-old pregnant woman in Wisconsin died of pneumonia as a complication of swine influenza.
A 1976 outbreak of swine influenza in Fort Dix, New Jersey, involved more than 200 cases, some of them severe, and one death.2 The first discovered case involved a soldier at Fort Dix who complained of feeling weak and tired. He died the next day.
The fear of an influenza pandemic in 1976 led to a national campaign in the United States designed to immunize nearly the entire population. In October, 1976, approximately 40 million people received the A/NewJersey/1976/H1N1 vaccine (ie, swine flu vaccine) before the immunization initiative was halted because of the strong association between the vaccine and Guillain-Barré syndrome (GBS).3,4 About 500 cases of GBS were reported, with 25 deaths due to associated pulmonary complications.5
A recent investigation sought to determine the link between GBS and the 1976 swine flu vaccine, since subsequent influenza vaccines did not have this strong association. Nachamkin et al (2008) found that inoculation of the 1976 swine flu vaccine, as well as the 1991-1992 and 2004-2005 influenza vaccines, into mice prompted production of antibodies to antiganglioside (anti-GM1), which are associated with the development of GBS. They proposed that further research regarding influenza vaccine components is warranted to determine how these components elicit antiganglioside effects.6
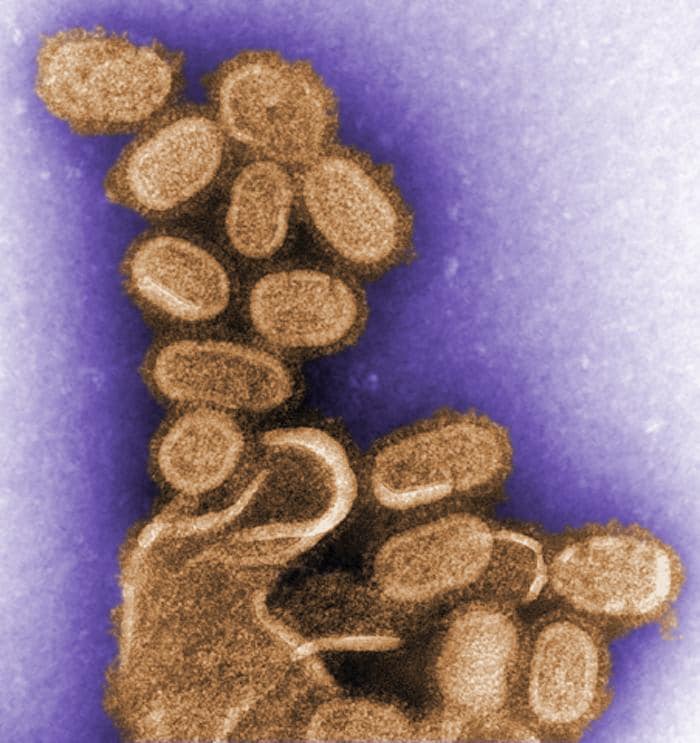
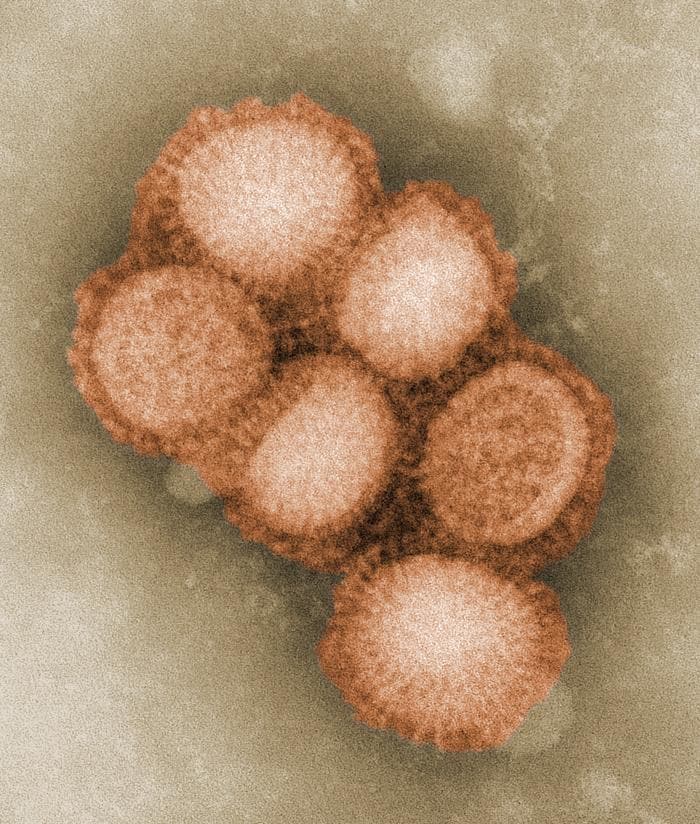
This preliminary negative stained transmission electron micrograph depicts some of the ultrastructural morphology of the A/CA/4/09 swine flu virus. Courtesy of CDC/ C. S. Goldsmith and A. Balish.
This preliminary negative stained transmission electron micrograph depicts some of the ultrastructural morphology of the A/CA/4/09 swine flu virus. Courtesy of CDC/ C. S. Goldsmith and A. Balish.
Current H1N1 influenza (formerly called swine influenza) outbreak
Human cases of influenza A (H1N1) have been reported worldwide. In 2009, cases of influenzalike illness were first reported in Mexico on March 18; the outbreak was subsequently confirmed as H1N1 influenza A.7 Investigation is continuing to clarify the spread and severity of H1N1 influenza (swine flu) in Mexico. Suspected clinical cases have been reported in 19 of the country's 32 states. Although only 97 of the Mexican cases have been laboratory-confirmed as Influenza A/H1N18 (12 of them genetically identical to Influenza A/H1N1 viruses from California7 ). As of May 5th, 2009, nearly 600 H1N1 influenza cases have been confirmed in Mexico, including 25 deaths.9
According to the WHO, as of May 4, 2009, H1N1 influenza had been laboratory-confirmed in 20 countries.8 For an updated tally of affected countries and counts, see WHO's Influenza A (H1N1) Web page. Cases are also suspected in Brazil.
On April 17, 2009, the CDC determined that two cases of febrile respiratory illness in children who resided in adjacent counties in southern California were caused by infection with a swine influenza A (H1N1) virus.10 By April 26, 2009, the US Department of Health and Human Services declared a national public health emergency involving H1N1 influenza A, citing its significant potential to affect national security.11 By May 5, 2009, more than 400 cases of H1N1 influenza had been confirmed in nearly all states within the United States and more than 1000 cases in 21 countries worldwide.8,12
For an updated tally and case counts in specific states, see the CDC's H1N1 Flu (Swine Flu) Web page. All affected patients have had mild influenzalike illness, with only two requiring brief hospitalization. As of May 1, 2009, only one death attributed to H1N1 flu had been reported in the United States, involving a 23-month-old child from Mexico who was visiting relatives in the United States.
Government and public health officials are monitoring this situation worldwide to assess the threat from H1N1 influenza and to provide guidance to health care professionals and the public. Because the situation is changing rapidly, it is important to check regularly for changes in recommendations as new information becomes available. Online resources for daily guidance include the Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), and Medscape's H1N1 Influenza A (Swine Flu) Alert Center.
Morbidity and Mortality
H1N1 influenza (swine flu) tends to cause high morbidity but low mortality rates (1%-4%).
Symptoms
Manifestations of H1N1 influenza (swine flu) are similar to those of seasonal influenza. Patients present with symptoms of acute respiratory illness, including at least 2 of the following:
- Fever
- Cough
- Sore throat
- Body aches
- Headache
- Chills and fatigue
- Diarrhea and vomiting (possible)
Persons with these symptoms should call their health care provider promptly. If an antiviral agent is warranted, it should ideally be initiated with 48 hours from the onset of symptoms (see Medications). The duration of illness is typically 4-6 days. The infectious period for a confirmed case is defined as 1 day prior to the onset of symptoms to 7 days after onset.
In children, signs of severe disease include apnea, tachypnea, dyspnea, cyanosis, dehydration, altered mental status, and extreme irritability.13
Viral Strain and Testing
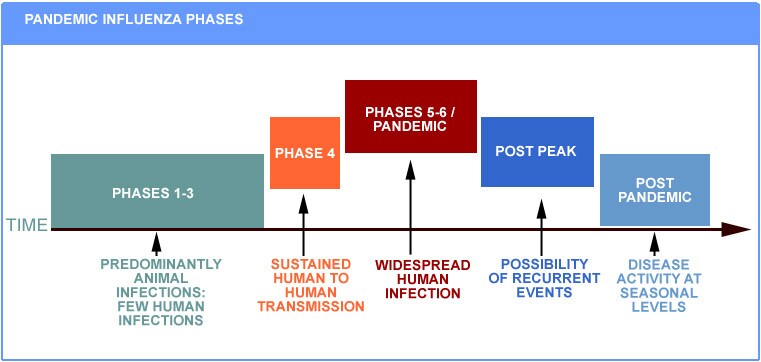
Outbreaks of H1N1 influenza (swine flu) are common in pigs year-round. Historically, when humans have become infected, it is a result of close contact with infected pigs (but not consumption of pork). However, the current virus is a novel influenza A (H1N1) virus not previously identified in humans, and it appears to be spread by human-to-human transmission. The WHO has raised its pandemic alert level for H1N1 influenza to phase 5, which is a strong signal that a pandemic is imminent and that the time to finalize the organization, communication, and implementation of the planned mitigation measures is short.
Phase 5 is characterized by human-to-human spread of the virus into at least two countries in one WHO region. While most countries will not be affected at this stage, the declaration of Phase 5 is a strong signal that a pandemic is imminent and that the time to finalize the organization, communication, and implementation of the planned mitigation measures is short. Courtesy of the WHO.
In the current 2009 outbreak in the United States, preliminary testing has shown that, in all cases, the viruses have the same genetic pattern. The virus is being described as a new subtype of influenza A/H1N1 not previously detected in pigs or humans.
Clinicians should consider the possibility of H1N1 influenza virus infections in patients who present with febrile respiratory illness. The CDC criteria for suspected H1N1 influenza are as follows14 :
- Onset of acute febrile respiratory illness within 7 days of close contact with a person who has a confirmed case of H1N1 influenza A virus infection, or
- Onset of acute febrile respiratory illness within 7 days of travel to a community (within the United States or internationally) where one or more H1N1 influenza A cases have been confirmed, or
- Acute febrile respiratory illness in a person who resides in a community where at least one H1N1 influenza case has been confirmed.
If H1N1 flu is suspected, the clinician should obtain a respiratory swab for H1N1 influenza testing and place it in a refrigerator (not a freezer). Once collected, the clinician should contact his or her state or local health department to facilitate transport and timely diagnosis at a state public health laboratory.
Laboratories should send all influenza A specimens that they are unable to subtype to the Viral Surveillance and Diagnostic Branch of the CDC's Influenza Division as soon as possible for further diagnostic testing.15
Viral tracking and research
Internationally, scientists have been collaborating on genetic analysis of current animal and human influenza viruses. These researchers have created a human/swine A/H1N1 influenza wiki to facilitate rapid dissemination of the results of this work. The collaboration is producing insights on the origin of the H1N1 virus and should enable scientists to track its evolution as the outbreak spreads around the world. Information from the National Institute of Allergy and Infectious Disease regarding influenza genome sequencing is available to researchers studying how influenza viruses evolve and those developing new and improved ways to prevent, diagnose, and treat influenza disease.16,17
Treatment Recommendations
Treatment is largely supportive and consists of bedrest, increased fluid consumption, cough suppressants, and antipyretics and analgesics (eg, acetaminophen, nonsteroidal anti-inflammatory drugs) for fever and myalgias. Severe cases may require intravenous hydration and other supportive measures. Antiviral agents may also be considered for treatment or prophylaxis (see Medications).
Patients should be encouraged to stay home if they become ill, to avoid close contact with people who are sick, to wash their hands often, and to avoid touching their eyes, nose, and mouth. The CDC recommends the following actions when human infection with H1N1 influenza (swine flu) is confirmed in a community13 :
Home isolation
- Patients who develop flulike illness (ie, fever with either cough or sore throat) should be strongly encouraged to self-isolate in their home for 7 days after the onset of illness or at least 24 hours after symptoms have resolved, whichever is longer.
- To seek medical care, patient should contact their health care providers to report illness (by telephone or other remote means) before seeking care at a clinic, physician's office, or hospital.
- Patients who have difficulty breathing or shortness of breath or who are believed to be severely ill should seek immediate medical attention.
- If the patient must go into the community (eg, to seek medical care), he or she should wear a face mask to reduce the risk of spreading the virus in the community when coughing, sneezing, talking, or breathing. If a face mask is unavailable, ill persons who need to go into the community should use tissues to cover their mouth and nose while coughing.
- While in home isolation, patients and other household members should be given infection control instructions, including frequent hand washing with soap and water. Use alcohol-based hand gels (containing at least 60% alcohol) when soap and water are not available and hands are not visibly dirty. Patients with H1N1 influenza should wear a face mask when within 6 feet of others at home.
Household contacts who are not ill
- Remain home at the earliest sign of illness.
- Minimize contact in the community to the extent possible.
- Designate a single household family member as caregiver for the patient to minimize interactions with asymptomatic persons.
School dismissal and childcare facility closure
- Strong consideration should be given to close schools upon a confirmed case of H1N1 flu or a suspected case epidemiologically linked to a confirmed case.
- Decisions regarding broader school dismissal within these communities should be left to local authorities, taking into account the extent of influenzalike illness within the community.
- Cancelation of all school or childcare related gatherings should also be announced.
- Encourage parents and students to avoid congregating outside of the school if school is canceled.
- Duration of schools and childcare facilities closings should be evaluated on an ongoing basis depending on epidemiological findings.
- Consultation with local or state health departments is essential for guidance concerning when to reopen schools. If no additional confirmed or suspected cases are identified among students (or school-based personnel) for a period of 7 days, schools may consider reopening.
- Schools and childcare facilities in unaffected areas should begin preparation for possible school closure.
Social distancing
- Large gatherings linked to settings or institutions with laboratory-confirmed cases should be canceled (eg, sporting events or concerts linked to a school with cases); other large gatherings in the community may not need to be canceled at this time.
- Additional social distancing measures are currently not recommended.
- Persons with underlying medical conditions who are at high risk for complications of influenza should consider avoiding large gatherings.
Patient education
Patients should be referred to the eMedicine Health article Swine Flu.
Preventive measures for health care personnel
The CDC has issued interim recommendations for controlling the spread of H1N1 influenza in health care settings.18 Recommended measures for care of patients with suspected or confirmed H1N1 influenza include the following:
- Place patients in a single-patient room with the door kept closed. An airborne-infection isolation room with negative-pressure air handling can be used, if available. Air can be exhausted directly outside or can be recirculated after filtration by a high efficiency particulate air (HEPA) filter.
- Suctioning, bronchoscopy, or intubation should be performed in a procedure room with negative-pressure air handling.
- Patients should wear a surgical mask when outside their room.
- Encourage patients to wash their hands frequently and to follow respiratory hygiene practices. Cups and other utensils used by the ill person should be washed with soap and water before use by other persons.
- Routine cleaning and disinfection strategies used during influenza seasons can be applied.
- Standard, droplet, and contact precautions should be used for all patient care activities and maintained for 7 days after illness onset or until symptoms have resolved.
- Health care personnel should wash their hands with soap and water or use hand sanitizer immediately after removing gloves and other equipment and after any contact with respiratory secretions.
- Personnel providing care to or collecting clinical specimens from patients should wear disposable nonsterile gloves, gowns, and eye protection (eg, goggles) to prevent conjunctival exposure.
- As per previous recommendations regarding mask and respirator use during influenza pandemics, personnel engaged in aerosol-generating activities (eg, collection of clinical specimens, endotracheal intubation, nebulizer treatment, bronchoscopy) and/or resuscitation involving emergency intubation or cardiac pulmonary resuscitation should wear a fit-tested disposable N95 respirator.
- Pending clarification of transmission patterns for the 2009 H1N1 influenza A (swine flu) virus, personnel providing direct patient care for suspected or confirmed cases should wear a fit-tested disposable N95 respirator when entering the patient's room.
H1N1 influenza in pregnancy
Pregnant women with suspected H1N1 influenza should receive empiric antiviral treatment.19
Medications
Laboratory testing has found the H1N1 influenza A (swine flu) virus susceptible to the prescription antiviral drugs oseltamivir and zanamivir, and the CDC has issued interim guidance for the use of these drugs to treat and prevent infection with swine influenza viruses.20,21 As part of its preparation for the emergency, the US Department of Homeland Security is releasing 25% of stockpiled antiviral agents (ie, oseltamivir [Tamiflu], zanamivir [Relenza]).
The usual vaccine for influenza administered at the beginning of the flu season is not effective for this viral strain. Also, other antiviral agents (eg, amantadine, rimantadine) are not recommended because of recent resistance to other influenza strains documented over the past several years.
Basic supportive care (ie, hydration, analgesics, cough suppressants) should be prescribed. Empiric antiviral treatment should be considered for confirmed, probable, or suspected cases of H1N1 influenza. Treatment of hospitalized patients and patients at higher risk for influenza complications should be prioritized.
Initiation of antiviral agents within 48 hours of symptom onset is imperative for providing treatment efficacy against influenza virus. In studies of seasonal influenza, evidence for benefits of treatment is strongest when treatment is started within 48 hours of illness onset. However, some studies of treatment of seasonal influenza have indicated benefit, including reductions in mortality or duration of hospitalization, even in patients in whom treatment was started more than 48 hours after illness onset. The recommended duration of treatment is 5 days.20,21
- Prophylaxis with antiviral agents should also be considered in the following individuals (pre-exposure or postexposure):
- Close household contacts of a confirmed or suspected case who are at high risk for complications (eg, chronic medical conditions, persons >65 y or <5>
- School children at high risk for complications who have been in close contact with a confirmed or suspected case
- Travelers to Mexico who are at high risk for complications (eg, chronic medical conditions, persons >65 y or <5>
- Health care providers or public health workers who were not using appropriate personal protective equipment during close contact with a confirmed or suspected case
- Pre-exposure prophylaxis can be considered in the following persons:
- Any health care provider who is at high risk for complications (eg, persons with chronic medical conditions, adults >65 y, pregnant women)
- Individuals not considered to be at high risk but who are nonetheless traveling to Mexico, first responders, or border workers who are working in areas with confirmed cases
Antiviral Agents
Drugs indicated for treatment of H1N1 influenza A virus include neuraminidase inhibitors (ie, oseltamivir and zanamivir).
Oseltamivir (Tamiflu)
Oseltamivir inhibits neuraminidase, which is a glycoprotein on the surface of influenza virus that destroys an infected cell's receptor for viral hemagglutinin. By inhibiting viral neuraminidase, this agent decreases the release of viruses from infected cells and, thus, viral spread. Oseltamivir is effective in the treatment of influenza A or B and must be administered within 48 hours of symptom onset to provide optimal treatment. The sooner the drug is administered after symptom onset, the better the likelihood of a good outcome. However, some studies of treatment of seasonal influenza have indicated benefit, including reductions in mortality or duration of hospitalization even for patients whose treatment was started more than 48 hours after illness onset.20 Oseltamivir reduces the length of illness by an average of 1.5 days. (In a subgroup of high-risk patients, illness was reduced by 2.5 d.) In addition, the severity of symptoms is also reduced.
Duration of administration for treatment is 5 days. Postexposure prophylaxis should be initiated within 7 d of exposure and continued for at least 10 days. Pre-exposure prophylaxis should be initiated during potential exposure period and continue for 10 days after last known exposure.20
Oseltamivir is available as 30-mg, 45-mg, and 75-mg oral capsules and as a powder for suspension that contains 12 mg/mL after reconstitution.
- Adult dose
- Treatment for acute illness: 75 mg PO bid for 5 d
- Prophylaxis: 75 mg PO qd (Please refer to duration of prophylaxis specific for postexposure.)
- Pediatric dose
- Treatment for acute illness and age <1 type="square">
- <3>
- 3-5 months: 20 mg PO bid for 5 d
- 6-11 months: 25 mg PO bid for 5 d
- Treatment for acute illness and age >1 year
- <15>
- 15-23 kg: 45 mg PO bid for 5 d
- 23-40 kg: 60 mg PO bid for 5 d
- >40 kg: Administer as in adults
- Prophylaxis and age <1 type="square">
- <3>
- 3-5 months: 20 mg PO qd
- 6-11 months: 25 mg PO qd
- <15>
- 15-23 kg: 45 mg PO qd
- 23-40 kg: 60 mg PO qd
- >40 kg: Administer as in adults
Zanamivir (Relenza)
Zanamivir inhibits neuraminidase, which is a glycoprotein on the surface of the influenza virus that destroys the infected cell's receptor for viral hemagglutinin. By inhibiting viral neuraminidase, release of viruses from infected cells and viral spread are decreased. Zanamivir is effective against both influenza A and B. The preparation of zanamivir is in powder form for inhalation via the Diskhaler oral inhalation device. Circular foil discs that contain 5-mg blisters of drug are inserted into the supplied inhalation device. Individuals with asthma or other respiratory conditions that may decrease ability to inhale drug should be given oseltamivir.
- Adult dose
- Treatment for acute illness: 10 mg inhaled orally bid for 5 d
- Prophylaxis of household contact: 10 mg inhaled orally qd for 10 d (initiate within 36 h)
- Prophylaxis for community outbreak: 10 mg inhaled orally qd for 28 d (initiate within 5 d of outbreak)
- Pediatric dose
- Treatment for acute illness
- <7>
- >7 years: Administer as in adults
- Prophylaxis in household contact
- <5>
- >5 years: Administer as in adults
- Prophylaxis in community outbreak
- Adolescents 12-16 years: Administer as in adults
- Treatment for acute illness
Additional pediatric considerations
Aspirin or aspirin-containing products (eg, bismuth subsalicylate [Pepto Bismol]) should not be included in the treatment of confirmed or suspected viral infection in persons aged 18 years or younger because of the risk of Reye syndrome. For relief of fever, other antipyretic medications (eg, acetaminophen, nonsteroidal anti-inflammatory drugs) are recommended.
Pregnant women
Oseltamivir and zanamivir are "Pregnancy Category C" medications, indicating that no clinical studies have been conducted to assess the safety of these medications in pregnant women.
Because of the unknown effects of influenza antiviral drugs on pregnant women and their fetuses, oseltamivir or zanamivir should be used during pregnancy only if the potential benefit justifies the potential risk to the embryo or fetus; the manufacturers' package inserts should be consulted. However, no adverse effects have been reported among women who received seltamivir or zanamivir during pregnancy or among infants born to women who have received oseltamivir or zanamivir.
Pregnancy should not be considered a contraindication to oseltamivir or zanamivir use. Because zanamivir is an inhaled medication and has less systemic absorption, some experts prefer zanamivir over oseltamivir for use in pregnant women, when feasible.20,22
Multimedia
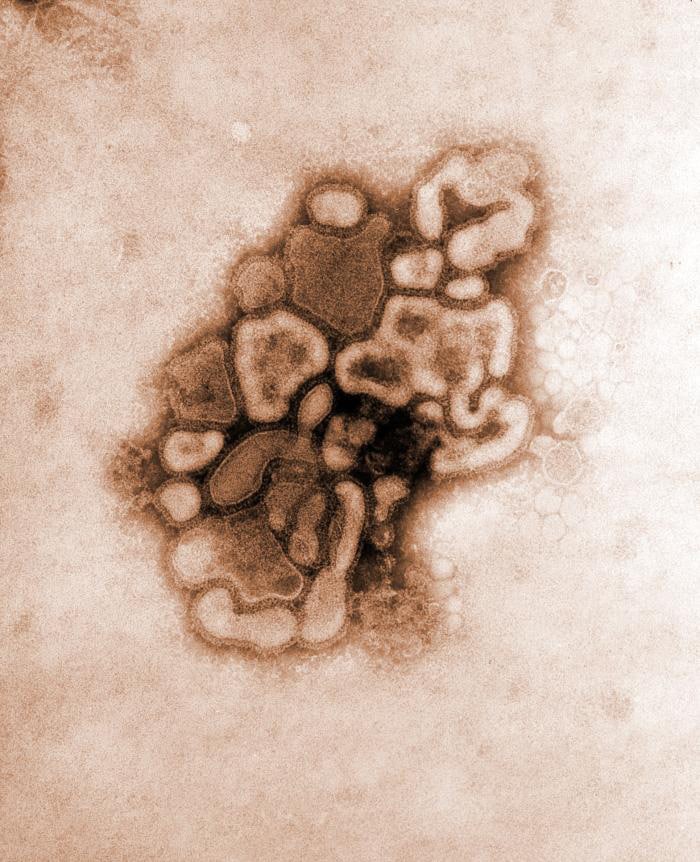
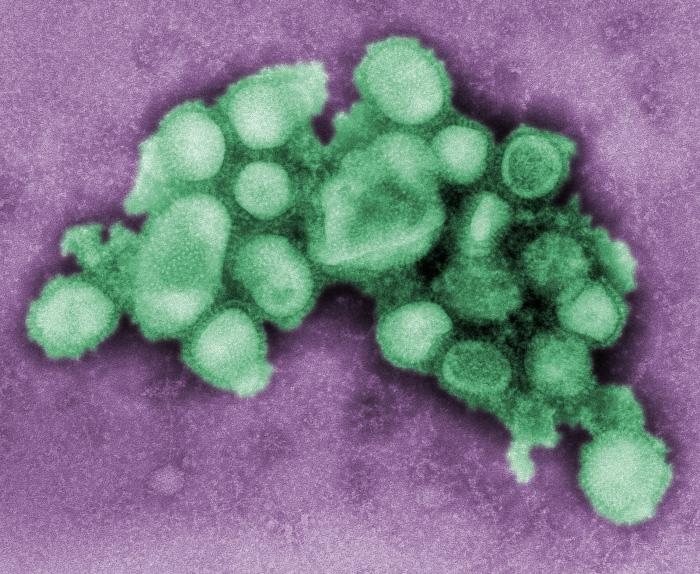
 | Media file 3: Negative stained transmission electron micrograph of recreated 1918 influenza virions. Courtesy of CDC/ Dr. Terrence Tumpey. |
Keywords
H1N1 influenza, H1N1 flu, swine flu, swine influenza, swine influenza virus, swine influenza A (H1N1) virus, human swine flu, influenza A, influenza (H1N1), SIV, swine flu symptoms, swine flu diagnosis, swine flu treatment, swine flu antiviral, swine flu pandemic, swine flu outbreak, H1N1 flu symptoms, H1N1 flu diagnosis, H1N1 flu treatment, H1N1 flu antiviral, H1N1 flu pandemic, H1N1 flu outbreak









No comments:
Post a Comment